
gonorrheais a deformity of the knee joint. It is accompanied by damage to the hyaline cartilage of the tibial and femoral articular surfaces and has a chronic progressive course. Clinical symptoms include pain that worsens with movement, limited movement, and synovitis (fluid buildup) in the joint. In later stages, support on the legs is reduced and movement is clearly limited. Pathology is diagnosed based on history, complaints, physical examination, and arthrograms. Conservative treatment: drug treatment, physical therapy, exercise. If the joint is significantly destroyed, arthroscopy is indicated.
General information
Arthritis (from the Latin genus articulatio - knee joint) or deforming arthropathy of the knee joint is a progressive degenerative-dystrophic lesion of the cartilage in the joint of a non-inflammatory nature. Gonorrhea is the most common arthritis. Usually affects middle-aged and elderly people, women are more commonly affected. After trauma or continuous high-intensity stress (for example, when playing professional sports), gonorrhea can occur at a younger age. Prevention plays the most important role in preventing the occurrence and development of gonorrhea.
Contrary to popular belief, the cause of the development of the disease does not lie in salt deposition, but in malnutrition and changes in the structure of intra-articular cartilage. With gonorrhea, calcium salt deposits can occur at the attachment sites of the tendons and ligamentous apparatus, but they are secondary and do not cause painful symptoms.
Cause of gonorrhea
In most cases, it is not possible to identify any reasons for the development of pathology. As a rule, the appearance of gonorrhea is due to a combination of several factors, including:
- Injury. About 20-30% of cases of gonorrhea are associated with previous injuries: tibial fractures (especially intra-articular), meniscal injuries, torn or ruptured ligaments. Usually, gonorrhea occurs 3-5 years after the injury, although the disease can develop earlier - 2-3 months after the injury.
- Do exercise. Most often, manifestations of gonorrhea are associated with excessive load on the joints. The age after 40 is the period when many people understand that regular physical activity is necessary to maintain the body in good condition. When starting to exercise, they do not take into account age-related changes and create unnecessary loads on the joints, which leads to the rapid development of degenerative changes and the appearance of symptoms ofgonorrhea. Running and squatting fast and at high intensity are especially dangerous for the knee joints.
- Overweight. With excess body weight, the load on the joints increases, both microtrauma and severe damage (torn meniscus or torn ligaments) occur more often. Gonorrhea is especially difficult in obese patients with severe varicose veins.
The risk of gonorrhea is also increased after previous arthritis (psoriatic arthritis, reactive arthritis, rheumatoid arthritis, gouty arthritis or ankylosing spondylitis). In addition, risk factors for the development of gonorrhea include hereditary weakness of the ligamentous apparatus, metabolic disorders and neurological deficits in certain neurological diseases, traumatic brain injury and trauma. Spine.
Pathogenesis
The knee joint is formed by the articular surfaces of two bones: the femur and the tibia. On the front surface of the joint is the patella, which, when moving, slides along the depression between the condyles of the femur. The fibula does not participate in the formation of the knee joint. Its upper part is located next to and just below the knee joint and is connected to the tibia through a low-motion joint.
The articular surfaces of the tibia and femur, as well as the posterior surface of the patella, are covered with smooth, very strong and elastic hyaline cartilage 5-6 mm thick. Cartilage reduces friction during movement and performs the function of absorbing shock when subjected to impact loads.
In the early stages of gonorrhea, blood circulation in small blood vessels that nourish hyaline cartilage is disrupted. The cartilage surface becomes dry and gradually loses its smoothness. Cracks appear on its surface. Instead of sliding smoothly, unhindered, the cartilage "clings" to each other. Due to constant microtrauma, cartilage tissue becomes thinner and loses its shock-absorbing properties.
In the second stage of gonorrhea, compensatory changes occur in the bone structure. The common platform is flattened, adapting to increased loads. The subchondral area (the bone just below the cartilage) thickens. Bone growths appear along the edges of the joint surfaces - bone spurs, which look like spurs on an X-ray.
During the process of gonorrhea, the synovial membrane and joint capsule also degenerate and become "wrinkled". The nature of the joint fluid changes - it thickens, viscosity increases, which leads to a deterioration of its lubricating and nutritional properties. Due to lack of nutrients, cartilage degeneration occurs faster. The cartilage becomes thinner and in some areas completely disappears. After the cartilage disappears, friction between joint surfaces increases sharply and degeneration occurs rapidly.
In the third stage of gonorrhea, the bones are significantly deformed and seem to be pressed against each other, significantly limiting joint mobility. Cartilage tissue is practically absent.
Classify
Taking into account the pathogenesis in trauma and orthopedics, two types of gonorrhea are distinguished: primary (idiopathic) gonorrhea and secondary gonorrhea. Primary gonorrhea occurs without previous trauma in elderly patients and is often bilateral. Secondary gonorrhea develops based on pathological changes (disease, developmental disorders) or injury to the knee joint. Can occur at any age, usually unilaterally.
Taking into account the severity of pathological changes, three stages of gonorrhea are distinguished:
- Early stage- initial manifestations of gonorrhea. Characterized by periodic dull pain, usually after heavy loading of the joint. There may be mild swelling in the joint that goes away on its own. There is no distortion.
- Second stage- Increased symptoms of gonorrhea. The pain becomes longer and more intense. A crunching sound often appears. There is a mild or moderate limitation of motion and mild deformity of the joint.
- Third stage– Clinical manifestations of gonorrhea reach their maximum level. The pain is almost constant, gait is impaired. There is marked limitation of mobility and notable deformity of the joint.
Symptoms of gonorrhea
The disease begins gradually, gradually. In the early stages of gonorrhea, patients feel slight pain when moving, especially when going up or down stairs. There may be a feeling of stiffness and "tightness" in the popliteal area. A characteristic symptom of gonorrhea is "starting pain" - a painful feeling that occurs during the first steps after getting up from a sitting position. When a patient with gonorrhea "diverges", the pain decreases or disappears, and after significant stress it appears again.
The outside of the knee remains unchanged. Sometimes patients with gonorrhea notice slight swelling in the affected area. In some cases, at the initial stages of gonorrhea, fluid accumulates in the joints - synovitis develops, characterized by an increase in the volume of the joint (swollen, spherical), a feeling of heaviness andlimit movement.
In the second stage of gonorrhea, the pain becomes more intense, occurs even with light loads and intensifies with intense or long walks. As a rule, the pain is localized along the anterior inner surface of the joint. After a long period of rest, the pain often disappears and reappears with movement.
As gonorrhea progresses, the range of motion of the joint gradually decreases, and when trying to bend the leg as much as possible, sharp pain appears. There may be a crunching sound when moving. The shape of the joint changes, as if it is expanding. Synovitis appears more often in the early stages of gonorrhea and is characterized by a more persistent course and more fluid accumulation.
In the third stage of gonorrhea, the pain becomes almost constant, making the patient uncomfortable not only when walking but also when resting. In the evening, patients take a long time to find a comfortable position to sleep. Often the pain appears even at night.
Flexion at the joint is significantly limited. In some cases, not only the ability to flex, but also the ability to extend is limited, which is why patients with gonorrhea cannot straighten their legs completely. Joints are enlarged and deformed. Some patients develop hallux valgus or varus deformities - the legs become X- or O-shaped. Due to limited movement and deformity of the legs, the gait becomes unstable and waddling. In severe cases, patients with gonorrhea can only move with the support of a cane or crutches.
Diagnose
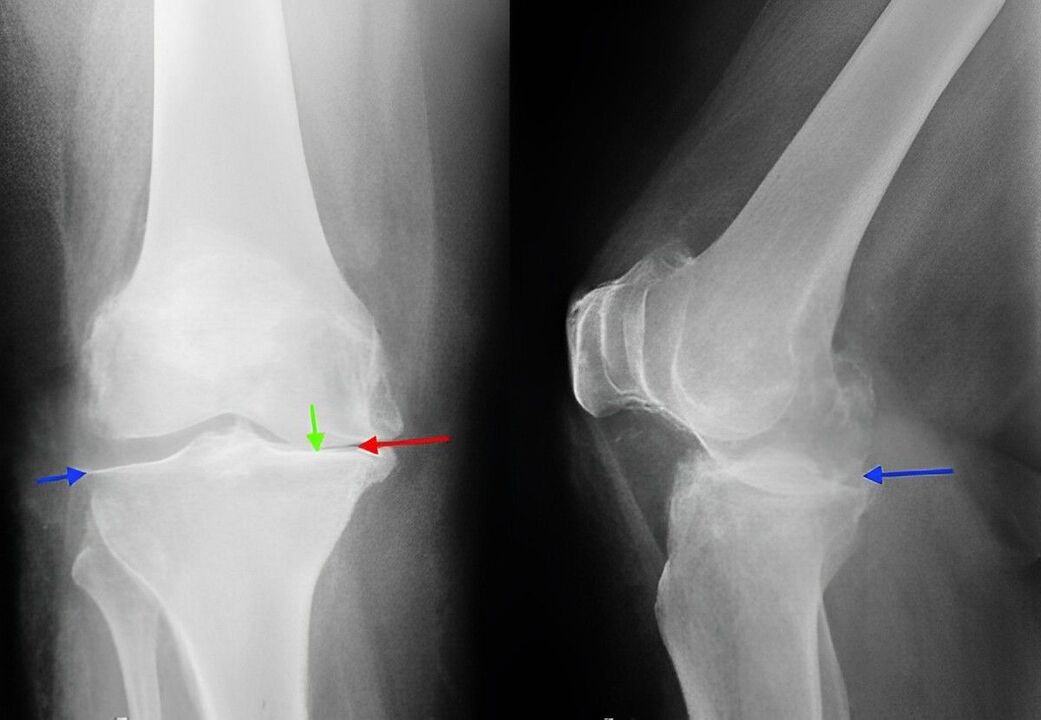
Diagnosis of gonorrhea is made based on patient complaints, objective examination data and x-ray examination. When examining a patient with gonorrhea in the early stages, it is often impossible to detect external changes. In the second and third stages of gonorrhea, the contours of the bones become rough, deformation of the joints, restriction of movement and curvature of the axis of the limb. When the patella moves in a horizontal direction, you will hear a crunching sound. Palpation will reveal the painful area from the inside of the patella, at the level of the joint, as well as above and below it.
With synovitis, the joint increases in volume, its contours become smooth. A bulge was detected along the anterolateral surface of the joint and above the patella. On palpation, fluctuations are determined.
X-ray of the knee joint is a classic technique that allows you to clarify the diagnosis, determine the severity of pathological changes in gonorrhea and monitor the course of the process, taking repeated picturesAfter a while. Due to its availability and low cost, it remains the primary method for diagnosing gonorrhea to this day. In addition, this research method allows to exclude other pathological processes (for example, tumors) in the tibia and femur.
In the early stages of gonorrhea, radiographic changes may be absent. Then, narrowing of the joint space and compaction of the subchondral area are determined. The ends of the femoral joints and especially the tibia are stretched, the condylar edge is sharp.
When studying radiography, it should be borne in mind that more or less pronounced changes characteristic of gonorrhea are observed in most elderly people and are not always accompanied by pathological symptoms. The diagnosis of gonorrhea is made only when there is a combination of radiological and clinical signs of the disease.
Currently, along with traditional radiography, modern techniques such as computed tomography of the knee joint, which allows detailed study of pathological changes in the bone structure, and MRI of the knee joint, are used toidentifies changes in soft tissue, used to diagnose gonorrhea. .
Treatment of gonorrhea
Conservative activity
Treatment is performed by traumatologists and orthopedists. Treatment for gonorrhea should start as soon as possible. During periods of exacerbation, patients with gonorrhea should rest to maximize joint relief. The patient is prescribed therapeutic exercises, massage, physiotherapy (UHF, electrophoresis with novocaine, phonophoresis with hydrocortisone, electrodynamic current, magnetic and laser therapy) and mud therapy.
Drug treatment for gonorrhea includes chondroprotective drugs (drugs that improve joint metabolism) and joint fluid replacement drugs. In some cases, with gonorrhea, injections of steroid hormones into the joint are prescribed. The patient may then be transferred to a nursing home for treatment.
Patients with gonorrhea may be advised to walk with a cane to reduce the load on the joints. Sometimes special orthotics or custom insoles are used. To slow down the degenerative process in the joints with gonorrhea, it is very important to follow certain rules: exercise, avoid unnecessary stress on the joints, choose comfortable shoes, monitor weightheavy, rationally organize your daily routine (alternate load and rest, perform special exercises).
Surgery
With pronounced destructive changes (in the third stage of gonorrhea), conservative treatment is ineffective. In case of severe pain, joint dysfunction and limited ability to function, especially if young or middle-aged patients have gonorrhea, surgery (knee replacement) is required. After that, recovery measures are taken. Full recovery time after joint replacement surgery due to gonorrhea takes from 3 months to 6 months.





































